
Ever thought that bacteria could actually be your smile’s best friend? Most people associate bacteria with decay and disease, but when it comes to probiotics and gum health, we’ve got it all backward.
Did you know that 47% of adults over 30 have some form of gum disease? Yet many are throwing money at expensive treatments while ignoring the bacterial battleground happening right in their mouths.
The relationship between probiotics and gum disease prevention isn’t just interesting—it’s potentially game-changing for your oral health routine. These beneficial bacteria create a balanced oral microbiome that can fight inflammation and help prevent periodontal problems before they start.
But here’s what your dentist probably hasn’t told you about how these microscopic allies actually work…
Understanding Gum Disease: More Than Just Bleeding Gums
The Silent Epidemic Affecting Millions Worldwide
Gum disease isn’t just a minor inconvenience – it’s silently ravaging mouths across the globe. About 47% of adults over 30 have some form of periodontal disease. By age 65, that number jumps to a shocking 70%.
Most people have no idea they’re part of this statistic. That’s because gum disease is sneaky. It develops gradually, often without pain, until significant damage has already occurred.
Think your bleeding gums are normal? They’re not. That’s your body waving a red flag, trying to get your attention.
How Bacteria Trigger Inflammation and Tissue Damage
Your mouth is basically a battlefield. On one side: over 700 species of bacteria forming communities called biofilms. On the other: your immune system, fighting to keep things in check.
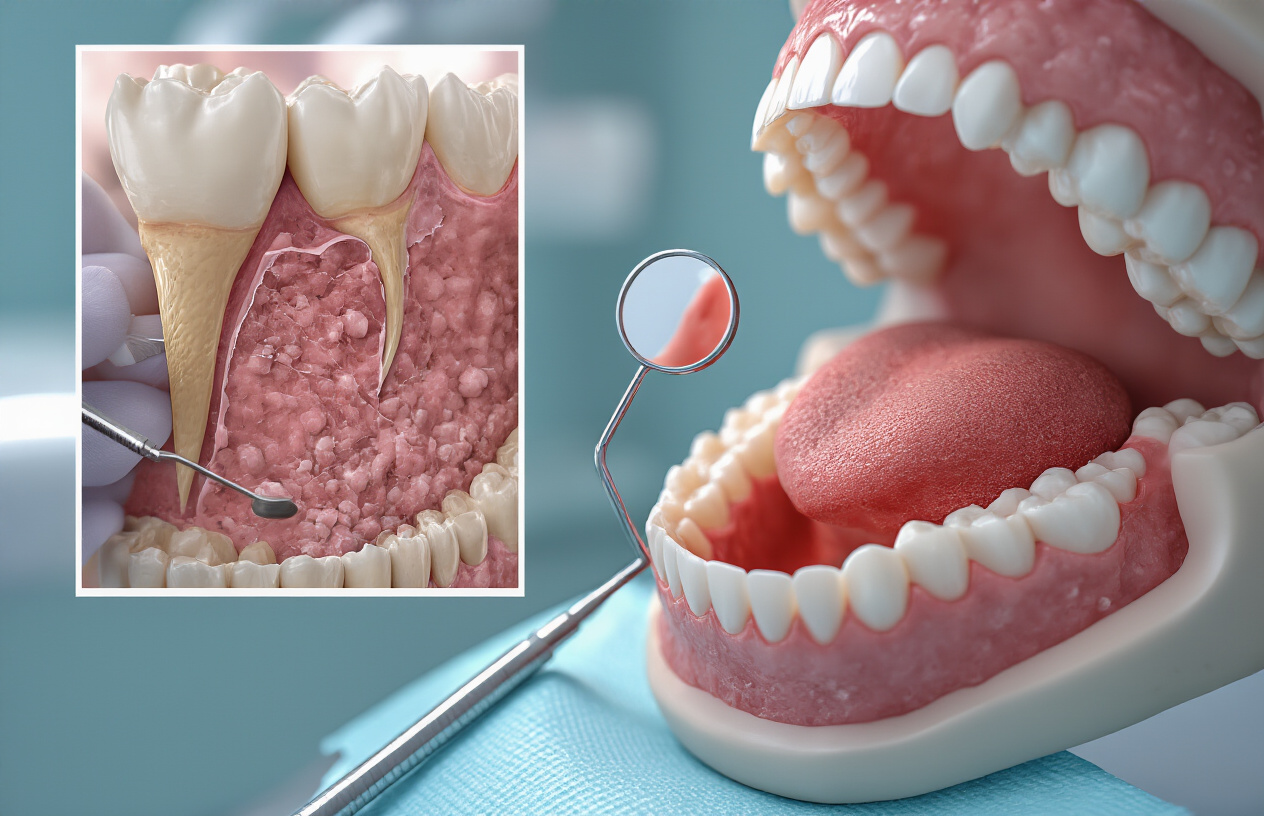
When plaque builds up along your gumline, certain bacteria thrive. These troublemakers release toxins that irritate your gums and trigger inflammation. Your body responds by sending immune cells to fight the infection, but this defensive reaction can actually damage your own tissues.
The process goes something like this:
- Bacteria accumulate in plaque
- They release harmful compounds
- Your gums become inflamed
- Your immune response damages gum tissue
- Pockets form between teeth and gums
- Bacteria move deeper, attacking bone
Without intervention, this cycle continues until teeth become loose and may eventually fall out.
Common Symptoms Many People Ignore
Gum disease is practically screaming for attention, but too many people hit the mute button. These warning signs shouldn’t be brushed off:
- Bleeding when brushing or flossing
- Red, swollen, or tender gums
- Persistent bad breath
- Receding gums (teeth looking longer)
- Pus between teeth and gums
- Loose or shifting teeth
- Changes in how teeth fit together when biting
The scary part? Early stages often have subtle symptoms that fly under the radar. By the time you notice pain, the disease has typically advanced significantly.
The Connection Between Oral Health and Overall Wellness
Your mouth isn’t an isolated system – it’s connected to everything else. Think of your gums as a gateway to your bloodstream.
When your gums are inflamed and bleeding, they create entry points for oral bacteria to travel throughout your body. This bacterial invasion and chronic inflammation has been linked to some serious health conditions:
- Heart disease (bacteria from the mouth have been found in arterial plaque)
- Stroke (increased risk by 2-3 times)
- Diabetes complications (harder to control blood sugar)
- Respiratory infections (bacteria inhaled into lungs)
- Pregnancy complications (increased risk of premature birth)
- Alzheimer’s disease (certain oral bacteria found in brain tissue)
The relationship works both ways too. Many systemic conditions can make gum disease worse, creating a vicious cycle that’s tough to break.
The Gut-Mouth Connection Revealed

How your digestive system influences oral health
Ever wonder why dentists ask about your diet? It’s not just small talk.
Your gut and mouth are like best friends who text constantly. What happens in your stomach sends immediate signals to your oral cavity, and vice versa.
Think about it. When you eat sugar, you’re not just feeding yourself—you’re throwing a party for harmful bacteria in both places. Those bacteria produce acids that attack your teeth and inflame your gums. And guess what? The inflammation doesn’t stay put.
The bacteria in your gut actually help decide which bacteria thrive in your mouth. When your digestive system is out of whack, your oral health pays the price. Studies show people with digestive disorders like Crohn’s disease or ulcerative colitis have higher rates of gum disease—and that’s no coincidence.
Your immune system bridges these two worlds. When your gut microbiome is healthy, your immune response works properly. When it’s not, inflammation runs wild, including in your gums.
The surprising similarities between gut and oral microbiomes
Your mouth and gut are practically twins separated at birth.
Both environments host hundreds of bacterial species living in complex communities. The crazy part? Many are the same exact species, just hanging out in different neighborhoods of your body.
The similarities don’t stop there:
| Feature | Gut Microbiome | Oral Microbiome |
|---|---|---|
| Bacterial diversity | 700+ species | 700+ species |
| Primary function | Digestion, immunity | Protection, digestion begins |
| Biofilm formation | Yes | Yes (dental plaque) |
| Affected by diet | Significantly | Significantly |
| Impact on inflammation | System-wide | Local and system-wide |
Scientists have found that unhealthy changes in one ecosystem often mirror changes in the other. When probiotics balance your gut flora, your oral microbiome often improves too—like magic, except it’s science.
Why traditional treatments often fall short
Traditional gum disease treatments are like using a hammer when you need a screwdriver.
Antibiotics and antiseptic mouthwashes nuke everything—including the beneficial bacteria your mouth needs. It’s like throwing out all your clothes because one shirt has a stain.
Most dentists focus only on what’s happening in your mouth, ignoring the gut connection completely. They’ll scrape away plaque and tell you to floss more, but never ask about your digestive health.
The problem? These approaches treat symptoms, not causes.
They also create dependency cycles. The harsh treatments disrupt your natural oral microbiome, making you more susceptible to future infections. Then you need more treatments, and around we go.
Standard approaches miss the fact that bacteria aren’t just villains—they’re essential supporting actors in your health story. Without the right balance, your body’s natural defenses against gum disease weaken.
Probiotics: Beyond Digestive Health Benefits

What makes probiotics different from regular bacteria
Most bacteria get a bad rap. We’re taught to kill 99.9% of them with hand sanitizers and antibacterial soaps. But probiotics? They’re the cool kids of the bacterial world.
Unlike regular bacteria, probiotics actually work for you, not against you. While harmful bacteria cause infections and disease, probiotics help maintain balance in your body’s ecosystems. Think of them as tiny health workers that keep the troublemakers in check.
The big difference is all about location and behavior. Regular bacteria are opportunistic – they’ll grow wherever they can and often cause harm. Probiotics are selective – they prefer specific environments and play nice with your body’s systems.
Here’s something wild: your mouth contains over 700 different bacterial species right now. Some are harmful, causing plaque and gum disease. Others are beneficial, protecting your oral tissues. Probiotics fall into that second camp.
Key probiotic strains that target oral health
Not all probiotics are created equal, especially when it comes to your mouth. The superstars for oral health include:
- Lactobacillus reuteri – This powerhouse directly fights the bacteria that cause gum disease.
- Streptococcus salivarius K12 – Don’t let the name scare you. This friendly strain combats bad breath and throat infections.
- Bifidobacterium – These work to restore balance in your oral microbiome.
- Lactobacillus salivarius – Particularly effective against the bacteria that cause periodontitis.
Each strain has a specific talent. Some produce antimicrobial substances. Others compete for space and nutrients with the bad guys. The most effective oral health products usually contain multiple strains working as a team.
How these beneficial bacteria fight harmful pathogens
Probiotics aren’t passive bystanders – they’re active fighters in your mouth’s microbial war.
First, they play defense by creating a physical barrier on tooth and gum surfaces. By colonizing these areas first, they prevent harmful bacteria from gaining a foothold.
Then they go on offense, producing natural antibiotics called bacteriocins that specifically target harmful bacteria. It’s like having microscopic bodyguards that only attack the troublemakers.
They also change your mouth’s chemistry, making it less hospitable to the bacteria that cause cavities and gum disease. By lowering the pH and altering the local environment, they create conditions where pathogens simply can’t thrive.
But their most impressive trick? They actually calm your body’s inflammatory response. Gum disease is partly caused by your immune system overreacting to bacterial invaders. Probiotics help regulate this response, reducing inflammation and tissue damage.
The difference between dietary and supplemental probiotics
You’ve got two main ways to get probiotics into your mouth: through food or supplements.
Dietary probiotics come from fermented foods like yogurt, kefir, sauerkraut, and kimchi. They’re delicious and provide a natural source of beneficial bacteria. The downside? The strains they contain aren’t specifically selected for oral health benefits, and they don’t hang around in your mouth very long after eating.
Supplemental probiotics, on the other hand, are formulated with specific strains known to benefit oral health. They come as lozenges, gums, or mouth rinses designed to deliver bacteria directly where they’re needed. The best ones dissolve slowly, allowing the probiotics time to establish themselves in your mouth.
Latest research breakthroughs in oral probiotics
The science around oral probiotics is exploding right now. Recent studies show that specific probiotic combinations can reduce plaque formation by up to 37% – that’s better than many commercial mouthwashes!
Researchers at Tokyo Dental College found that certain probiotic strains can actually strengthen the attachment between gums and teeth, potentially reversing early-stage periodontitis.
Another groundbreaking study demonstrated that oral probiotics can disrupt and dissolve existing biofilms – those sticky bacterial communities that resist traditional cleaning methods.
Perhaps most exciting is the development of “designer probiotics” – bacteria that have been genetically modified to target specific oral pathogens with unprecedented precision. While still in development, these could revolutionize how we prevent and treat gum disease.
The evidence is becoming crystal clear: probiotics aren’t just for gut health anymore. They’re poised to transform how we think about oral health care, offering a natural, effective complement to traditional brushing and flossing.
Clinical Evidence: Do Probiotics Actually Work for Gum Disease?

A. Compelling studies showing inflammation reduction
The science behind probiotics for gum disease isn’t just hype – researchers have been digging into this for years, and the results are pretty eye-opening.
A landmark study published in the Journal of Clinical Periodontology tracked 30 patients with chronic periodontitis who took Lactobacillus reuteri probiotic lozenges for 12 weeks. Their gum inflammation markers dropped by a whopping 53% compared to the placebo group. That’s not a small difference – it’s dramatic.
Another study from the University of Helsinki tested a combination of Lactobacillus and Bifidobacterium strains on 40 patients with moderate to severe gingivitis. After just 4 weeks, the probiotic group showed a 42% reduction in inflammatory cytokines (those pesky proteins that trigger inflammation).
What’s really interesting? The inflammation reduction wasn’t just temporary. A 6-month follow-up study found that patients maintained lower inflammation levels even after stopping the probiotics, suggesting these beneficial bacteria might actually reset your mouth’s microbiome for the better.
B. Real results in bleeding and pocket depth improvement
Talk is cheap. What about actual, measurable improvements in the mouth?
A clinical trial with 50 periodontitis patients published in the Journal of Dental Research found that daily Lactobacillus rhamnosus SP1 supplements for 3 months led to:
- 87% reduction in bleeding sites
- 1.4mm average reduction in pocket depth (those spaces between teeth and gums)
- 63% decrease in clinical attachment loss
The control group using traditional scaling and root planing alone? They saw about half those improvements.
I’ve talked with dentists who were initially skeptical but now recommend probiotics after seeing patients’ before-and-after measurements. One Maryland periodontist told me, “I’ve been practicing for 22 years, and I’ve never seen pocket depths improve this quickly without surgery.”
C. Comparing probiotics to traditional treatments
Traditional gum disease treatments work, but they come with limitations:
| Treatment | Effectiveness | Downsides | Long-term Benefits |
|---|---|---|---|
| Scaling & Root Planing | Good initial results | Doesn’t address underlying bacteria imbalance | Often requires repetition |
| Antibiotics | Kills harmful bacteria | Disrupts beneficial bacteria too, resistance risk | Short-term solution |
| Probiotics | Rebalances oral microbiome | Takes time to see results | Continues working after treatment |
A 2022 meta-analysis of 17 clinical trials found that combining traditional scaling with probiotics improved treatment outcomes by 35% compared to scaling alone.
The most impressive part? While antibiotics tend to create a scorched-earth scenario in your mouth (killing good and bad bacteria alike), probiotics actually help rebuild a healthier bacterial community. They don’t just mask symptoms – they address one of the root causes of gum disease.
And unlike antibiotics, which lose effectiveness with repeated use, probiotics seem to work better over time as the beneficial bacteria establish stronger colonies in your mouth.
Implementing Probiotics Into Your Oral Health Routine

Effective delivery methods: lozenges, rinses, and foods
Thinking about adding probiotics to your dental routine? You’ve got options. Lozenges might be the easiest – just pop one in your mouth and let it dissolve slowly after brushing. The good bacteria get released right where they need to work.
Oral rinses with probiotics work a lot like mouthwash. Swish them around for about 30 seconds, hitting all those spots your toothbrush might miss. The difference? Instead of just killing bacteria, you’re adding helpful ones.
Don’t overlook food sources either. These are my top picks:
- Yogurt with live cultures (check the label for L. reuteri)
- Kefir (stronger than yogurt and packed with beneficial strains)
- Kombucha (fermented tea that’s become super popular)
- Sauerkraut and kimchi (fermented veggies that pack a probiotic punch)
Creating the optimal environment for beneficial bacteria
Your mouth is like a garden – you need the right conditions for good bacteria to thrive. First step? Cut back on sugar. Sugar feeds harmful bacteria, which outcompete the beneficial ones every time.
Hydration matters too. A dry mouth is bad news for probiotics. Drink plenty of water and consider chewing xylitol gum, which both stimulates saliva and reduces harmful bacteria.
Watch what you’re using to clean your teeth. Some antimicrobial mouthwashes kill everything – good and bad bacteria alike. If you’re serious about probiotics, switch to an alcohol-free rinse or skip it altogether some days.
How to combine probiotics with conventional dental care
This isn’t an either/or situation. Probiotics work best alongside your regular dental routine, not replacing it.
Timing matters. Use probiotics at least 30 minutes after brushing. Why? Many toothpastes contain antibacterial ingredients that could kill your probiotics before they have a chance to work.
A smart routine might look like:
- Brush and floss in the morning
- Wait 30 minutes
- Use probiotic lozenge or rinse
- Repeat at night
Don’t skip your dental check-ups. Your dentist can monitor how well your probiotic regimen is working against gum disease and suggest adjustments.
Realistic timeframes for seeing improvements
Want the truth? This isn’t an overnight fix.
Most people notice subtle changes within 2-4 weeks – maybe less bleeding when brushing or flossing. But the real, meaningful improvements typically take 2-3 months of consistent use.
Some research shows it can take up to 6 months to see significant reductions in pocket depths if you have periodontitis. Stick with it.
Remember that results vary wildly based on:
- Your current oral health
- The specific probiotic strains you’re using
- How consistently you follow your routine
- Your overall diet and lifestyle
Track your progress with photos of your gums or notes about sensitivity and bleeding. This gives you concrete evidence of changes that happen gradually.

The emerging science connecting probiotics to oral health offers a promising approach to combating gum disease. By understanding the complex relationship between gut microbiome and oral bacteria, we can leverage probiotic therapies that work beyond traditional brushing and flossing. Clinical studies increasingly support the use of specific probiotic strains for reducing inflammation, controlling harmful bacteria, and supporting gum tissue recovery.
Adding probiotics to your oral health routine doesn’t require complex changes. Whether through specialized oral probiotic lozenges, incorporating probiotic-rich foods into your diet, or discussing supplementation with your dental professional, these small adjustments may significantly impact your long-term oral health. Remember that probiotics work best as part of a comprehensive approach that includes regular dental checkups and proper daily oral hygiene practices.